News
Celebrating progress in palliative care: 10 years since the resolution
Palliative care is not just a service, but a lifeline for families navigating challenging health experiences.
Living with a life-limiting or life-threatening condition involves navigating significant changes, including managing symptoms and side effects. This experience can be overwhelming for families. However, palliative care teams provide essential support and guidance, helping to ease the journey during these difficult times.
The World Health Organisation defines palliative care as the prevention and relief of suffering of adult and paediatric (child) patients and their families, facing the problems associated with life-threatening and life-limiting illnesses. Globally, an estimated 56.8 million people are in need of palliative care.
In the Western Cape, healthcare workers throughout the public system, ranging from tertiary hospitals to regional and district facilities, as well as primary and community healthcare, work together to provide comprehensive care to all people for a wide range of diseases, including chronic diseases such as cardiovascular diseases, cancer, chronic respiratory diseases, AIDS, and diabetes. Many other conditions may require palliative and hospice care, including kidney failure, chronic liver disease, multiple sclerosis, Parkinson’s disease, rheumatoid arthritis, neurological disease, dementia, congenital anomalies, and drug-resistant tuberculosis. Services include addressing the physical, psychological, social, and spiritual needs of patients and family members.
This October, the Western Cape Department of Health and Wellness proudly celebrates World Hospice and Palliative Care Day. The Department hosted its annual Palliative Care Day celebration at the Red Cross War Memorial Children’s Hospital on 10 October 2024, ahead of World Hospice and Palliative Care Day on 12 October 2024. This year also marks 10 years since the World Health Assembly passed 2014 World Health Assembly (WHA) Resolution 67.19 on Palliative Care, calling for all countries to “strengthen palliative care as a component of comprehensive care throughout the life course”.
Western Cape Minister of Health and Wellness, Mireille Wenger, reaffirmed the department’s commitment to palliative care. “Palliative care is more than managing symptoms; it’s about honouring the human experience and ensuring that every person receives compassionate care tailored to their needs. Our department is committed to strengthening palliative care services to enhance the quality of life for children and adults who require this specialised service. I also want to take this opportunity to thank our dedicated healthcare teams who provide this service with compassion and care.”
Red Cross War Memorial Children’s Hospital is a dedicated child health institution and offers a comprehensive range of specialist paediatric services to children, including a dedicated palliative care service launched in 2023. In an effort to strengthen paediatric palliative care, the hospital announced its draft Paediatric Palliative Care Framework at the yearly event, which emphasises a holistic, multidisciplinary approach. This framework is designed to support children and their families facing life-limiting or life-threatening illnesses, ensuring that they receive continuous, compassionate care throughout their healthcare journey. Hospital management hopes to see this model adopted in children’s wards and hospitals throughout the country.
Dr Anita Parbhoo, CEO at the Red Cross War Memorial Children’s Hospital, reflected on the hospital’s commitment to providing palliative care to all children and their families. “The hospital strives to work together to give each child an opportunity to live the most fulfilled life possible. For many children who receive care here, it means a long, fruitful life. For other children, however, it is about the team providing the child and the family with a dignified, pain free and peaceful death. This framework seeks to set out the ways of working to ensure that the holistic needs of the child and family are explored and addressed. This can only be done by a multidisciplinary team who connects and brings together their collective wisdom to develop a care plan to care for and meet the expectations of the patient and family.”
Other strides made by the department in palliative care include offering specialised training for healthcare providers to enhance skills in delivering services to adults and children. This included increasing the budget to address training needs.
Palliative care training is crucial for healthcare workers . This training teaches professionals how to communicate effectively, making it easier to discuss difficult topics like prognosis and treatment options with sensitivity. It also focuses on managing symptoms, which greatly improves patients’ quality of life.
In a paediatric setting, for instance, a trained palliative care team or nurse can offer valuable support for a child diagnosed with cancer. A palliative care nurse works collaboratively with oncologists and other healthcare providers to manage the child’s symptoms, such as pain or nausea, while also providing psychological and emotional support for the child and their family. They might organise family meetings to discuss treatment plans, focusing on the child’s quality of life and the family’s preferences. Additionally, the palliative care team may provide counselling or refer the family to a social worker to navigate the challenges of the diagnosis. This integrated approach fosters a supportive environment for children and their families.
Elrien Joubert, Clinical Training Manager for the department, shares: “Recent enhancements in palliative care training have marked a significant step forward in professional development across the healthcare community. With an increased training budget, we’ve seen a substantial rise in attendance and demand for programmes that cater to a diverse audience, ensuring that all healthcare providers are equipped with the skills necessary to deliver compassionate care. Feedback from training surveys highlights an overwhelmingly positive experience among participants, indicating not only satisfaction but also notable professional growth. These improvements reflect our commitment to elevating palliative care practices, ultimately benefiting patients and families in need of comprehensive support.”
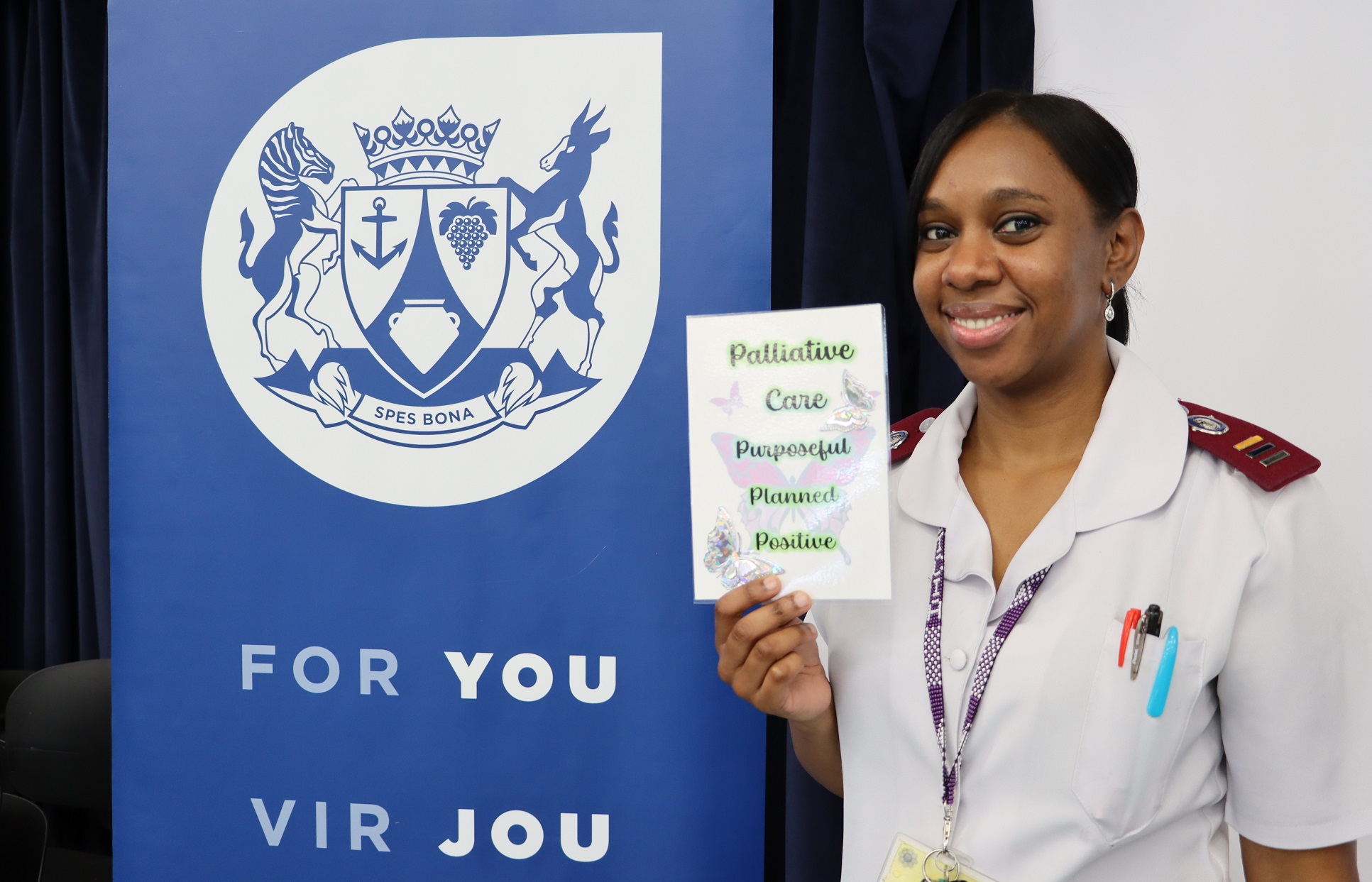
Registered professional nurse Alicia Dauds leads the palliative care service in collaboration with other healthcare workers at the Red Cross War Memorial Children’s Hospital. Nurse Dauds says her training has strengthened her ability to support both the patients and their families during challenging times. “For me, I didn’t choose to be a palliative care nurse, I feel like palliative care chose me. As a palliative care nurse, I build relationships with our young patients and their families who need support following a diagnosis. We often find that families don’t open up easily – but as palliative care nurses, we build relationships and walk a difficult journey with them. Part of my job includes counselling, either individual counselling with the patient or group counselling with the family. I also work closely with our doctors to ensure that families better understand the next steps of a patient’s care and how the family can provide support and be supported.”
The Western Cape Department of Health and Wellness remains committed to collaborating with its partners to ensure that no one is left behind. We strive to provide essential palliative care through qualified professionals whenever it is needed. As we reflect on a decade since the resolution, we are reminded of the progress made and the work that still lies ahead to improve the quality of life for all our citizens. We call on all people and stakeholders to raise awareness on palliative care and support those in need.





